Knee & Hip Replacement
- Home
- Knee & Hip Replacement
Knee Replacement: Regain Mobility and Live Pain-Free
Expert Joint Replacement by Dr. Debabrata Padhy
Are you struggling with joint pain while walking, climbing stairs, or doing daily activities?
Do you have osteoarthritis, a joint injury, or stiffness that limits your movement?
If yes, knee or hip replacement surgery may be the right solution for you.
Dr. Debabrata Padhy is one of the most trusted orthopedic surgeons in Bhubaneswar, known for his expertise in joint replacement surgeries, especially knee and hip replacements. With years of experience and a compassionate approach, he has helped hundreds of patients regain their independence and lead pain-free lives.
At his clinic, patients receive personalised evaluation and advanced surgical care focused on long-term joint health and improved mobility.
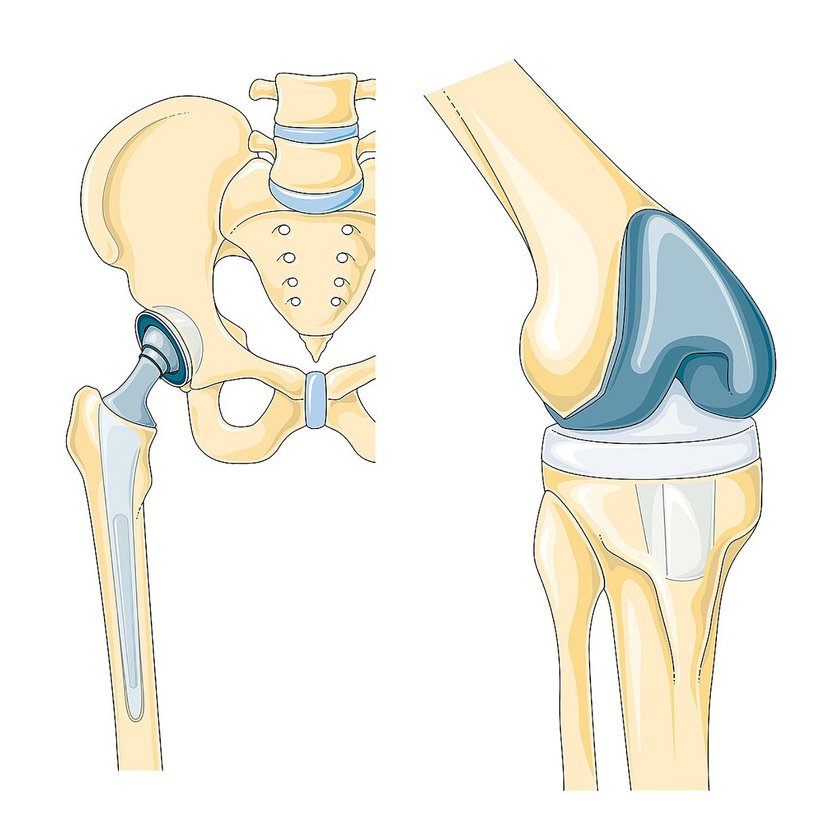
Knee Replacement Surgery
Who Needs Knee Replacement?
Who Needs Knee Replacement?
- Persistent knee pain that affects daily life
- Osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis
- Limited movement and swelling in the knee
- Knee injuries or cartilage damage
- Poor response to medications or physiotherapy
Benefits of Knee Replacement
- Relieves long-term knee pain
- Restores joint flexibility and movement
- Makes walking and daily activities easier
- Improves overall quality of life
- Helps you regain confidence and independence
Hip Replacement Surgery
What Is Hip Replacement?
Who Needs Hip Replacement?
- Chronic hip pain that limits walking or sitting
- Hip stiffness and reduced range of motion
- Arthritis or hip joint degeneration
- Hip injury, fractures, or avascular necrosis
- Helps you regain confidence and independence
- No relief from medications or lifestyle changes
Specification of Knee & Hip Replacement
The preoperative evaluation generally includes a review of all medications being taken by the patient. Anti-inflammatory medications, including aspirin, are often discontinued one week prior to surgery because of the effect of these medications on platelet function and blood clotting. Other preoperative evaluations include complete blood counts, electrolytes (potassium, sodium, chloride), blood tests for kidney and liver functions, urinalysis, chest X-ray, EKG, and a physical examination. Your physician will determine which of these tests are required, based on your age and medical conditions. Any indications of infection, severe heart or lung disease, or active metabolic disturbances such as uncontrolled diabetes may postpone or defer total hip joint surgery.
Total hip joint replacement can involve blood loss. Patients planning to undergo total hip replacement often will donate their own (autologous) blood to be stored for transfusion during the surgery. Should blood transfusion be required, the patient will have the advantage of having his or her own blood available, thus minimizing the risks related to blood transfusions.
Benefits of Hip Replacement
- Eliminates hip pain and discomfort
- Improves walking and standing balance
- Enhances mobility and flexibility
- Restores sleep and overall comfort
- Supports return to an active lifestyle
Before and During The Surgery
Before the Surgery
- Detailed medical evaluation
- X-rays, scans, and physical examination
- Personalized discussion of symptoms and treatment options
During the Surgery
- Performed under spinal or general anesthesia
- Damaged bone and cartilage are carefully removed
- An artificial joint (metal/plastic) is placed for smooth movement
- Surgical site is tested and securely closed
Recovery and Aftercare
Recovery and Aftercare
- Hospital stay: 2–3 days
- Physiotherapy starts within 24 hours post-surgery
- Pain managed with prescribed medications
- Full recovery: 4–6 weeks (varies per patient)
When Can I Resume Normal Activities?
- Light household work: 3–4 weeks
- Driving: 4–6 weeks (based on control and comfort)
- Walking, swimming, cycling: After full recovery
- Avoid: High-impact activities and sports involving jumps or jerks
Risks and How We Manage Them
- Blood clots
- Infection
- Nerve or tissue damage
- Joint stiffness
Why Choose Dr. Debabrata Padhy for Joint Replacement in Bhubaneswar?
- 20 years of experienced orthopedic surgeon.
- Patient-first approach with customised treatment.
- Advanced surgical techniques.
- Focus on quicker recovery and long-term mobility.
- Trusted by patients across Odisha.
- He has performed 5000+ joint replacement surgeries.
